CH Baktawar Singh Rd, Medicity, Islampur Colony, Sector 38, Gurugram, Haryana 122001

Myasthenia gravis is a chronic autoimmune, neuromuscular disease that causes weakness in the skeletal muscles that worsens after periods of activity and improves after periods of rest. These muscles are responsible for functions involving breathing and moving parts of the body, including the arms and legs.
The name myasthenia gravis, which is Latin and Greek in origin, means “grave, or serious, muscle weakness.” There is no known cure, but with current therapies, most cases of myasthenia gravis are not as “grave” as the name implies. Available treatments can control symptoms and often allow people to have a relatively high quality of life. Most individuals with the condition have a normal life expectancy.
Myasthenia gravis affects both men and women and occurs across all racial and ethnic groups. It most commonly impacts young adult women (under 40) and older men (over 60), but it can occur at any age, including childhood.
Myasthenia gravis is an autoimmune disease, which means the immune system—which normally protects the body from foreign organisms—mistakenly attacks itself.
Myasthenia gravis is caused by an error in the transmission of nerve impulses to muscles. It occurs when normal communication between the nerve and muscle is interrupted at the neuromuscular junction—the place where nerve cells connect with the muscles they control.
Neurotransmitters are chemicals that neurons, or brain cells, use to communicate information. Normally when electrical signals or impulses travel down a motor nerve, the nerve endings release a neurotransmitter called acetylcholine that binds to sites called acetylcholine receptors on the muscle. The binding of acetylcholine to its receptor activates the muscle and causes a muscle contraction.
In myasthenia gravis, antibodies (immune proteins produced by the body’s immune system) block, alter, or destroy the receptors for acetylcholine at the neuromuscular junction, which prevents the muscle from contracting. This is most often caused by antibodies to the acetylcholine receptor itself, but antibodies to other proteins, such as MuSK (Muscle-Specific Kinase) protein, also can impair transmission at the neuromuscular junction.
The thymus gland controls immune function and may be associated with myasthenia gravis. It grows gradually until puberty, and then gets smaller and is replaced by fat. Throughout childhood, the thymus plays an important role in the development of the immune system because it is responsible for producing T-lymphocytes or T cells, a specific type of white blood cell that protects the body from viruses and infections.
In many adults with myasthenia gravis, the thymus gland remains large. People with the disease typically have clusters of immune cells in their thymus gland and may develop thymomas (tumors of the thymus gland). Thymomas are most often harmless, but they can become cancerous. Scientists believe the thymus gland may give incorrect instructions to developing immune cells, ultimately causing the immune system to attack its own cells and tissues and produce acetylcholine receptor antibodies—setting the stage for the attack on neuromuscular transmission.
Rarely, mothers with myasthenia gravis have children who are born with myasthenia gravis (neonatal myasthenia gravis). If treated promptly, children generally recover within two months after birth.
Some children are born with a rare, hereditary form of myasthenia gravis, called congenital myasthenic syndrome.
The main symptom of MG is weakness in the voluntary skeletal muscles, which are muscles under your control.
The failure of muscles to contract usually happens because they can’t respond to nerve impulses. Without proper transmission of the impulse, the communication between nerve and muscle is blocked and weakness results.
Weakness associated with MG usually gets worse with more activity and improves with rest. Symptoms of MG may present.
MG can cause dropping of the eyelids, as well as double or blurry vision. You may also experience overall weakness in your eye muscles.
In addition to facial paralysis, MG may lead to changes in your facial expressions.
When MG affects the muscles of the throat, you may experience:
When MG affects the muscles of the chest area, you may experience severe and potentially life threatening symptoms:
Respiratory failure, caused by weakness in the diaphragm and chest muscles that may lead to myasthenic crisis and is considered an emergency
MG can also affect the muscles in your arms and legs, leading to the following symptoms:
Not everyone will have every symptom, and the degree of muscle weakness can change from day to day. The severity of the symptoms typically increases over time if left untreated.
A myasthenic crisis is a medical emergency that occurs when the muscles that control breathing weaken to the point where individuals require a ventilator to help them breathe. It may be triggered by infection, stress, surgery, or an adverse reaction to medication. Approximately 15 to 20 percent of people with myasthenia gravis experience at least one myasthenic crisis. However, up to one-half of people may have no obvious cause for their myasthenic crisis. Certain medications have been shown to cause myasthenia gravis. However, sometimes these medications may still be used if it is more important to treat an underlying condition.
A doctor may perform or order several tests to confirm the diagnosis of myasthenia gravis:
Because weakness is a common symptom of many other disorders, the diagnosis of myasthenia gravis is often missed or delayed (sometimes up to two years) in people who experience mild weakness or in those individuals whose weakness is restricted to only a few muscles.
Myasthenia gravis (MG) can be treated with drugs, surgery and other therapies – alone or in combination.
Myasthenia gravis treatment also includes self-care: getting plenty of sleep, resting your eyes, pacing your activity, eating healthy foods, exercising, and managing your stress.
There are two types of medications used to treat MG. One group—anticholinesterases—temporarily relieves the symptoms of MG. Another group—immunosuppressants—attacks the disease at its source. By suppressing the body’s immune system, these drugs stop the body from damaging the neuromuscular junction in the first place. Immunosuppressant treatments can have serious side effects.
Doctors may prescribe one or a combination of these medications. It often takes time to determine the best medication and dosage for an individual patient.
This is typically the first type of medication prescribed because it is has the fewest long-term side effects. It also is the most rapid-acting medication available. These drugs prevent the breakdown of acetylcholine—the chemical messenger that causes a muscle contraction. More acetylcholine generally results in greater muscle strength. Although anticholinesterase medication does not directly counteract the abnormal immune system attack in MG, they may partially or completely control myasthenia gravis symptoms in some patients.
The most commonly prescribed medication of this type is pyridostigmine bromide (Mestinon). It’s available in tablet or liquid, and comes in a time-release form. The different forms vary in how soon and how long they’re effective.
Acetylcholinesterases can cause stomach cramps and diarrhea; it helps to take them with bland food like crackers, applesauce or yogurt. Other common side effects include muscle twitching, muscle cramps and sweatiness. Sometimes these symptoms appear when too much medication is taken. If you have these symptoms, you should talk with your doctor to see if you should reduce your dose or vary when you take the medication.
Immunosuppressants help prevent your body from producing the harmful antibodies that cause MG weakness in the first place. At the same time, they also reduce the body’s production of good antibodies—which makes you more susceptible to infection and other diseases. While you’re taking immunosuppressants, it’s important to avoid people with contagious diseases. You may need to avoid crowds and wash your hands often.
The use of these medications must be monitored carefully by a physician because they may cause major side effects.
Prednisone significantly relieves MG symptoms for a large majority of those with myasthenia. This drug is not as fast acting as anticholinesterases, but it is faster than other immunosuppressants, and it is relatively inexpensive. It resembles natural hormones produced by the cortex of the human adrenal gland. While prednisone can be very effective in treating myasthenia, it carries the risk of serious side effects; their severity depends on the dosage and length of time prednisone is used. These include insomnia, mood changes, weight gain, fluid retention, reduced resistance to infection, increased susceptibility to diabetes, high blood pressure, osteoporosis, glaucoma, cataracts, and stomach ulcers, plus a host of other less common side effects. Most of these side effects can be prevented or managed with other medication. It also is very important to “eat healthy,” following a well-balanced diet that is high in potassium and calcium and low in sodium, fat, and cholesterol. This can help prevent bone thinning, reduce fluid retention, and minimize weight gain, for starters. When you take prednisone, it stops the body’s natural production of adrenal hormones. Prednisone therapy must not be stopped suddenly; the dose must be tapered gradually to “reawaken” the body’s natural hormones.
Other immunosuppressant medications. There are a number of other medications used to treat MG. Many were developed initially for organ transplant patients, or for treating other immune-related diseases. These include azathioprine (Imuran), mycophenylatemofetil (CellCept), tacrolimus (Prograf), methotrexate, cyclosporine (Sandimmune, Neoral), and cyclophosphamide (Cytoxan, Neosar). If one of these medications helps a person who has myasthenia, its use can eliminate the need for prednisone, or allow a lowering of its dose. These medications are complicated to administer. They can take months to become effective, the dosage varies from person to person, and each drug has its own side effects and drug interactions. Your doctor should go through the details of these medications with you.
Monoclonal antibody therapies. These newer, and very expensive, therapies target very specific components of the immune system. Rituximab (Rituxan) is given as a series of IV infusions every six months, and is especially effective in the MuSK variant of MG. The treatment suppresses the immune system by reducing B-lymphocytes. Eculizumab (Soliris) is used for generalized MG, and is given as a series of four weekly infusions followed by every two week administration. This treatment prevents the immune system from damaging the neuromuscular junction, requires special precautions, and may be used together with other treatments.
Immune globulin therapy can be used to treat rapidly worsening MG. Immune globulin is a human blood product pooled from multiple donors who are carefully screened. By providing the body with normal antibodies from donated blood, IVIg treatments appear to temporarily modify the immune system. For most individuals, MG weakness typically improves within a week of treatment and lasts for several weeks or months. IVIg treatments are expensive and offer short-term relief from Myasthenia gravis symptoms until longer acting immune modifying treatments are effective.
Side effects—for instance, headache or allergic symptoms–are usually related to how fast the drug is administered. Slowing the infusion rate can help with this. IVIg infusions are sometimes repeated at monthly intervals to sustain the treatment effect.
Plasmapheresis, or “plasma exchange,” is a procedure that removes antibodies—both “bad” and “good”—from the blood. Over several hours, blood is gradually removed through a special intravenous line, plasma which contains antibodies is separated off, and then the antibody-free blood is returned to the body along with a blood product called albumin to replace some of the proteins lost in the procedure. This treatment doesn’t affect the body’s ability to make more antibodies, and so the relief it provides is generally temporary. It also is expensive.
Plasmapheresis is used for patients who have severe myasthenia gravis symptoms, or who need to improve strength before surgery. It’s also used periodically for those who don’t respond to other treatments. With plasma exchange, an individual typically gets stronger in several days; the treatment benefit usually lasts two to three weeks. Since the effects are often short-term, a series of treatments over a period of two weeks is usually necessary.
Plasmapheresis involves removing large volumes of blood, which can lower the blood pressure and lead to dizziness or near-fainting. Allergic reactions – from fever, chills, and rash, to serious drops in blood pressure – may occur when donor blood products or plasma are given to the patient. This also may occur with administration of IV immune globulin.
Surgical treatment is thymectomy, removal of the thymus gland. This is the treatment for patients with thymomas, but is also considered for patients with MG who do not have thymomas.
The goal of a thymectomy is to remove the source of abnormal antibody production causing the disease thus leading to resolution of symptoms. The benefits of thymectomy are not realized immediately after surgery, thus patients will continue with their medical regimen after the procedure with the goal of weaning those medications over time. Individual response to thymectomy varies depending on the patient’s age, response to prior medical therapy, the severity of the disease and how long the patient has had myasthenia gravis.
Thymectomy is recommended for all patients with thymomas and for patients under 60 who have mild to moderate muscle weakness due to myasthenia gravis. Thymectomy generally is not used for treating patients with myasthenia gravis that affects only their eyes. Thymectomy appears to be most effective when it is performed six to 12 months after the onset of symptoms. It is important to talk to your doctor early in your diagnosis about thymectomy as an option for treatment.
Thymectomy can be performed by several different surgical techniques:
Transsternalthymectomy: In this procedure, the incision is made in the skin over the breastbone (sternum), and the breastbone is divided (sternotomy) to expose the thymus. This approach is commonly used for heart surgery. The surgeon removes the thymus through this incision as well as any residual fat in the center of the chest which may harbor extra thymic cells. This approach is commonly used when the patient has a thymoma.
Transcervicalthymectomy: In this procedure the incision is made across the lower part of the neck, just above the breastbone (sternum). The surgeon removes the thymus through this incision without dividing the sternum. This is mostly used in patients without thymoma with certain body-types.
Robotic thymectomy and video-assisted thorascopicthymectomy (VATS): These minimally invasive techniques use several tiny incisions in the chest. A camera is inserted through one of the incisions and the surgery is performed with video guidance. The surgeon removes the thymus by using special surgical tools inserted into the other incisions. In a robotic-assisted procedure, the surgeon uses robotic arms to perform the surgery. The goal is to provide the same result as the more invasive transsternal approach with less post-operative discomfort and a quicker recovery.
Complications of myasthenia gravis are treatable, but some can be life-threatening.
Myasthenic crisis is a life-threatening condition that occurs when the muscles that control breathing become too weak to work. Emergency treatment and mechanical assistance with breathing are needed. Medications and blood-filtering therapies help people to again breathe on their own.
Some people with myasthenia gravis have a tumor in the thymus gland, a gland under the breastbone that is involved with the immune system. Most of these tumors, called thymomas, aren't cancerous (malignant).
People with myasthenia gravis are more likely to have the following conditions:
At our center we do this surgery using VATS or the Da Vinci Robot and only small holes (1cm).
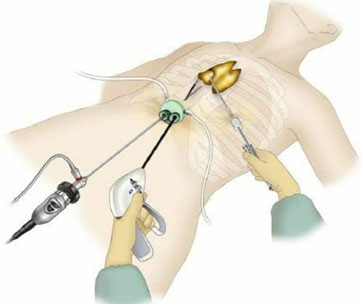
VATS Thymectomy

Ports for VATS Thymectomy
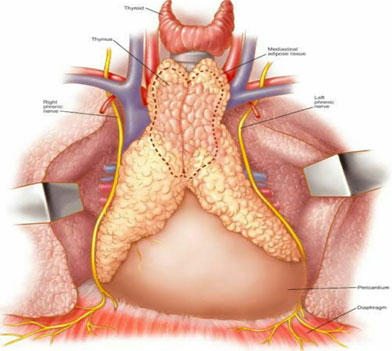
Thymus Gland and extent of Thymectomy