CH Baktawar Singh Rd, Medicity, Islampur Colony, Sector 38, Gurugram, Haryana 122001

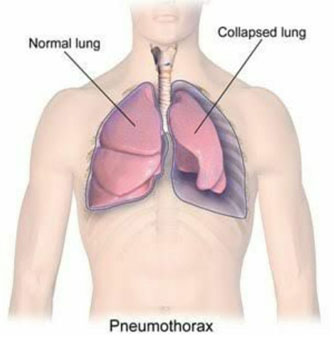
A pneumothorax is a collection of air outside the lung but within the pleural cavity. It occurs when air accumulates between the parietal and visceral pleurae inside the chest. The air accumulation can apply pressure on the lung and make it collapse. The degree of collapse determines the clinical presentation of pneumothorax. Air can enter the pleural space by two mechanisms, either by trauma causing communication through the chest wall or from the lung by rupture of the visceral pleura. A pneumothorax can be a complete lung collapse or a collapse of only a portion of the lung.
A pneumothorax can be caused by:
In general, men are far more likely to have a pneumothorax than women are. The type of pneumothorax caused by ruptured air blisters is most likely to occur in people between 20 and 40 years old, especially if the person is very tall and underweight.
Underlying lung disease or mechanical ventilation can be a cause or a risk factor for a pneumothorax. Other risk factors include:
Symptoms normally come on almost immediately and commonly begin with chest pain. Other signals that the problem may be a collapsed lung are:
Pneumothorax, sometimes referred to as a collapsed lung, is identified by a combination of diagnostic testing, physical examination, and medical history.
Dr. Harsh Vardhan Puri's thorough diagnostic technique will correctly identify pneumothorax and provide a suitable treatment strategy. Patients looking for the best care possible for complicated chest ailments and disorders turn to Dr. Puri because of his skill and commitment in maintaining his standing as a top authority on pneumothorax treatment in Gurgaon.
The treatment of pneumothorax depends on a number of factors, and may vary from discharge with early follow-up to immediate needle decompression or insertion of a chest tube. Treatment also depends on the physician that is going to handle the patient; pulmonary physicians usually perform medical thoracoscopy (minimally invasive) one port, while thoracic surgeons use a surgery suite and two ports. In some cases patient preference is requested.
In traumatic pneumothorax, chest tubes are usually inserted and these patients are handled by thoracic surgeons as other chest organs might be affected. If mechanical ventilation is required, the risk of tension pneumothorax is greatly increased and the insertion of a chest tube is mandatory. Any open chest wound should be covered with an airtight seal, as it carries a high risk of leading to tension pneumothorax.
Tension pneumothorax is usually treated with urgent needle decompression. There are several cases where “silent lung” is observed and needle decompression may be required before transport to the hospital upon the site of the accident, and can be performed by an emergency medical technician or other trained professional. The needle or cannula is left in place until a chest tube can be inserted. If tension pneumothorax leads to cardiac arrest, needle decompression is performed as part of resuscitation as it may restore cardiac output.
Small spontaneous pneumothoraces do not always require treatment, as they are unlikely to proceed to respiratory failure or tension pneumothorax, and generally resolve spontaneously. A case by case evaluation is needed and careful follow up of these patients. This approach is most appropriate if the estimated size of the pneumothorax is small (defined as <50% of the volume of the hemithorax), there is no breathlessness, and there is no underlying lung disease. A 24-hour observation is optional for these patients or clear instructions are given to return to hospital if there are worsening symptoms. Follow up as outpatients require repeated X-rays to confirm improvement. Secondary pneumothoraces are only treated conservatively if the size is very small (1 cm or less air rim) and there are limited symptoms. Oxygen given at a high flow rate may accelerate resorption as much as fourfold.
In view of a large PSP (>50%), or in a PSP associated with breathlessness, guidelines recommend that reducing the size by aspiration is equally effective as the insertion of a chest tube. In order to perform this procedure administration of local anesthetic is necessary and inserting a needle connected to a three-way tap; up to 2.5 liters of air (in adults). Upon follow up if there has been significant reduction in the size of the pneumothorax on subsequent X-ray, the remainder of the treatment can be conservative. It has been observed that when compared to tube drainage, first-line aspiration in PSP reduces the number of people requiring hospital admission significantly, without increasing the risk of complications. The same technique could be also considered in secondary pneumothorax of moderate size (air rim 1-2 cm) without breathlessness, however; ongoing observation in hospital is required even after a successful procedure.
A chest tube (or intercostal drain) is the most definitive initial treatment of a pneumothorax. Chest tube is typically inserted in an area under the axilla (armpit) called the “safe triangle”, where damage to internal organs can be avoided. Local anesthetic is applied. Usually there are two types of tubes used. In spontaneous pneumothorax, small-bore (smaller than 14 F, 4.7 mm diameter) tubes may be inserted by the Seldinger technique. Larger tubes do not have an advantage. It has been observed that for traumatic pneumothorax, larger tubes (28 F, 9.3 mm) are used.
Chest tubes are required in PSPs that have not responded to needle aspiration, in large SSPs (>50%), and in cases of tension pneumothorax. The method indicates that they are connected to a one-way valve system that allows air to escape, but not to re-enter, the chest. Several times it includes a bottle with water that functions like a water seal, or a Heimlich valve. Moreover; they are not usually connected to a negative pressure circuit, due to the fact that this would result in rapid re-expansion of the lung and a risk of pulmonary edema. The tube is left in place until no air is seen to escape from it for a period of time (no more than 2 days), and X-rays confirm re-expansion of the lung. If after 2-4 days there is still evidence of an air leak, various options are available. If air leak persists then, surgery may be required, especially in SSP.
Chest tubes are also used as first-line treatment when pneumothorax occurs in people with AIDS, usually due to underlying pneumocystis pneumonia (PCP), due to the fact that this condition is associated with prolonged air leakage. Furthermore, when bilateral pneumothorax occurs common in people with PCP, surgery is often required.
Pleurodesis is considered the final solution it is a procedure that permanently obliterates the pleural space and attaches the lung to the chest wall. Video Assisted Thoracic Surgery with identification of any source of air leakage and stapling of blebs—followed by pleurectomy of the outer pleural layer and pleural abrasion of the inner layer is considered most effective. During the healing process, the lung adheres to the chest wall, effectively obliterating the pleural space. Recurrence rates are approximately 1%. Post-thoracotomy pain is usually observed. The results of VATS are considered less effective than thoracotomy, however; smaller scars in the skin. VATS offers a shorter in-hospital stays, less need for postoperative pain control, and a reduced risk of lung problems after surgery. VATS may also be used to achieve chemical pleurodesis; this involves insufflation of talc. Insufflation of talc induces an inflammation of the pleura surfaces. If a chest tube is already in place, various agents may be instilled through the tube to achieve chemical pleurodesis, such as talc, tetracycline, minocycline or doxycycline. Results of chemical pleurodesis tend to be worse than when using surgical approaches, talc pleurodesis has been found to have the best results.
If pneumothorax occurs in a smoker, it may be advisable for someone to remain off work for up to a week after a spontaneous pneumothorax. For those who have undergone pleurodesis it may take up to two to three weeks off work to recover. Air travel is discouraged for up to seven days after complete resolution of a pneumothorax if recurrence does not occur. Underwater diving is considered unsafe after an episode of pneumothorax unless a preventative procedure has been performed. Currently professional guidelines suggest that pleurectomy should be performed on both lungs and that lung function tests and CT scan normalize before diving is resumed. Aircraft pilots may also require assessment for surgery.
Selecting Dr. Harsh Vardhan Puri for thoracic procedures such as pneumothorax treatment in Gurgaon is a choice based on knowledge, experience, and empathy. Dr. Puri is extremely knowledgeable and skilled, especially when it comes to treating thoracic operations.
His wealth of knowledge in treating various ailments guarantees that patients receive effective, individualized therapy that is catered to their individual need.
In addition, Dr. Puri is well known for his skill in handling challenging thoracic situations. His all-encompassing approach to care, together with cutting-edge surgical methods, guarantees the best possible results for his patients.
Apart from his proficiency in pneumothorax treatment in Gurgaon, Dr. Puri also possesses exceptional skills in minimally invasive techniques and robotic surgery. His proficiency in this extremely specialized area guarantees that patients get the best treatment possible from assessment to post-operative care during the transplant procedure.
Patients who select Dr. Harsh Vardhan Puri for Pneumothorax treatment in Gurgaon are certain to receive state-of-the-art care, individualized attention, and supportive guidance throughout their medical journey.
The location of the facility, the severity of the ailment, and the selected course of therapy all affect how much pneumothorax treatment costs in India. The price might vary from 50,000 rupees to 1,50,000 rupees on average. Speak to Dr. Harshvardhan Puri for affordable pneumothorax treatment in Gurgaon.
Thoracostomy, often known as chest tube insertion, is the emergency treatment for pneumothorax. By removing extra fluid or air from the area around the lung, this tube helps the lung expand once more and keeps it from collapsing further, enabling regular breathing to resume. To stabilise patients and enhance their results, Dr. Harshvardhan Puri offers complete emergent pneumothorax treatment in Gurgaon. He guarantees rapid diagnosis and intervention.
In most cases, pneumothorax surgery is safe when carried out by qualified physicians. Like any surgical operation, there are dangers involved, though, such as the possibility of bleeding, infection, anesthesia-related side effects, and harm to nearby structures.
Significant health hazards can result from pneumothorax, particularly if it fails to be treated or if problems develop. Pneumothorax primarily poses a danger of lung collapse, which can result in respiratory distress and reduced oxygenation. Untreated pneumothorax in extreme circumstances can develop into tension pneumothorax, a potentially fatal illness that has to be treated right once.
Small, simple pneumothoraxes sometimes heal on their own without requiring surgery. However, in order to avoid problems and encourage lung re-expansion, bigger or repeated pneumothoraces may need to be repaired surgically or by the insertion of a chest tube.
The severity of the illness, the method of treatment, and the patient's reaction to the medication all affect how long a patient must be in the hospital for a pneumothorax. Pneumothorax patients typically need to stay in the hospital for two to five days to be seen, treated, and have their lung re-expansion monitored.
Breathlessness, fast breathing, and quick onset chest discomfort are three prominent indicators of a collapsing lung (pneumothorax). A dry cough, chest tightness, a fast heartbeat, and cyanosis—a blue staining of the skin—may be further symptoms.